Systemic lupus erythematosus (SLE)
Keywords: Disseminated Lupus Erythematosus, other varieties- Acute cutaneous lupus, Chronic cutaneous lupus erythematosus, or discoid lupus erythematosus (DLE), Subacute cutaneous lupus erythematosus
What is Lupus?
Lupus erythematosus (SLE) is an autoimmune disease in which tissues and cells, including joints, skin, blood vessels and few organs like kidneys, etc., get damaged by antibodies generated in the patient’s own body. These antibodies get developed without any apparent reason, which is known to medical science. This disease is being increasingly reported in India.
Surprisingly, 90% of cases are seen in women, usually of child-bearing age, but children, men, and the elderly can be affected. Peak incidences are between 15 to 40 years of age group. Females: Male ratio varies from 09: 01 to 11: 01. However, SLE is less common in below 15years and above 40years of female age groups. In the United States, SLE is prevalent in urban areas, ranging from 15 to 50 per 100,000. Dark complexioned people are more affected. Hispanic and Asian populations are also susceptible.

Why does it happen?
Like most autoimmune diseases, the reason behind Lupus is not unknown; it is multifactorial, there are genetic characteristics that predispose specific individuals to SLE. And the other predisposing environmental factors might be ultraviolet light, drugs, foods, infections, etc. also play a role. These factors affect the female sex hormones and unknown neuroendocrine abnormalities. The results in abnormal immune responses release the pathogenic immunological autoantibodies, which causes tissue damage.
How does this damage happen?
As mentioned earlier, the tissue damage caused by pathogenic subsets of autoantibodies and immune complexes. The abnormal immune responses include
- Polyclonal and antigen-specific T and B lymphocyte hyperactivity
- Inadequate regulation of that hyperactivity.
These abnormal immune responses probably depend upon interactions between susceptibility genes and the environment.
- A defective or deleted class III allele, C4AQO, is the most common genetic marker associated with SLE in many ethnic groups.
- SLE associated with HLA-DR2 or DR3 in many groups, and single gene associations occur between HLA class 2 autoantibodies that associate with clinical subsets of Lupus.
- Environmental factors that cause flares of SLE are largely unknown, except for ultraviolet light. As many as 70% of patients become photosensitive, i.e., they become susceptible to daylight, which increases the symptoms like reddish rashes across the skin with itching, and burning.
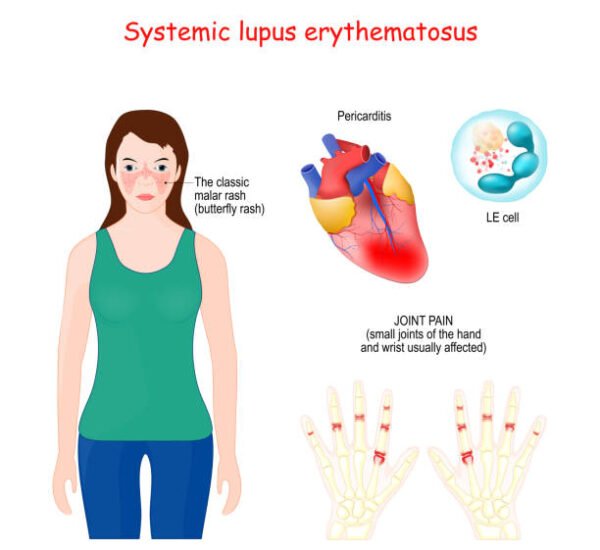
What are the clinical manifestations?
SLE involves every system in the body skin, blood, bones, kidneys, nervous system, cardiovascular system, etc.
The manifestations are:
- Arthritis
- Fever,
- Abdominal pain with nausea & vomiting
- Skin rash with photosensitivity
- Hairloss is a reasonably common
- Serositis
- Pleuritis
- Pericarditis
- Nephritis- loss of protein in urine leads to swelling and weight gain.
- Ulcers of the mouth (Oral ulcers)
- Raynaud’s phenomenon is when the blood supply to the fingers, toes, ears, nose is limited or interrupted or restricted, causing numbness.
- Neurological: neuro-psychiatrist, seizures, psychosis, organic brain syndrome, focal neurological disturbances, etc.
- Enlarged liver (Hepatomegaly) & Spleen (Splenomegaly)
- Subcutaneous nodules and Lymphadenopathy
- Cardiovascular manifestations- like valvular damage, pericarditis, ECG changes.
- Musculoskeletal involvement- arthralgia, myositis, bursitis, fascitis, carpal tunnel syndrome.
- Thrombocytopenia
What are the complications that happen?
Late-stage SLE shows much of the long-term complications.
- Disease complications- renal failure, stroke, heart attack, blood clotting, etc.
- Complications of the treatment are mainly related to painkillers like Nonsteroidal anti-inflammatory drugs (NSAID)- induced gastrointestinal complications.
- There may be various complications that arise due to the long-term use of corticosteroids, cytotoxic drugs.
How does the condition gets diagnosed?
The provisional diagnosis is made through the clinical features and involvement of different organs. Based on the clinical presentation and the suspicion few more tests are done. Though these blood tests are not conclusive, they indirectly lead to the diagnosis.
Following are the tests which are frequently done:
- Antinuclear antibodies (ANA) also known as immunofluorescent antinuclear antibody test. ANA test is reported in titers and patterns. However, we have to keep in mind that there may be people with negative ANA report but have SLE vice-versa; the people with positive ANA can also remain disease-free.
- Antidouble-stranded DNA antibody (Anti dsDNA)
- Anti-U1RNP antibodies
- Anti-Ro/SSA and Anti-La/SSB
- Anti-Histone Antibodies
- Antiphospholipid antibodies
Apart from these, the other screening tests like Complete blood count, Urine analysis, etc., also have significance in evaluating the individual’s stage and prognosis. If thesis positive insignificant titers, then the diagnosis is virtually confirmed. The presence of anti-dsDNA, patient-sm antibodies confirms the diagnosis. The biopsy is suggestible in renal involvement, otherwise, it is rarely indicated for diagnosis.
What to do? How do we manage Lupus?
The first step to manage Lupus is knowing the disease. We have to understand and accept the unpredictable nature of the disease and its curability. The treatment and outcome of the treatment are also very individualistic and vary from person to person.
- Education, counselling, and other psychological adaptation for the patients and family members are the most important.
- Patients with SLE should avoid exposure to the sun(ultraviolet rays ); going to hill stations may bring a relapse.
- Once the triggering factors are identified, one should avoid those precipitating factors.
- Mental and physical stress brings about a deterioration; reassurance with counsellors and daily light exercises may relieve these symptoms.
- A normal-balanced diet and low intake of salt.
- One should take precautions regarding pregnancy and birth control
- Better, one should avoid Estrogen-based birth control pills.
Other measures:
Since the reason behind the disease is not clearly understood, in modern medicine, the drugs usually prescribed to treat the inflammation and symptoms of SLE are Anti-inflammatory medications like NSAIDs or conventional painkillers, anti-malarial drugs, steroids like synthetic cortisone, and immunosuppressives (medications that suppress the immune system) etc. We all know that all these medications have potential side effects and should be consumed under strict monitoring and control. Numerous patients damage their vital organ functions due to the long-term consumption of these drugs. Hence be cautious.
How can “Let’s homoeopathy” help in cases of Lupus?
Homoeopathy works well for systemic lupus erythematosus. As mentioned earlier, the treatment approach for each patient with Lupus is very individual-oriented. The qualified doctors at Lets homoeopathy first carefully evaluate the constitution of the patient and his disease condition; after that, they suggest the best suitable medication, strength and dose for each of the individual patient.
At Let’s Homeopathy, we treat the person as a whole, not just targeting the symptoms, which means we treat the person and his pathological conditions together.
Remedies, as prescribed after case analysis, taking a history of the patient, family history, causation, emotional and physical stress and other factors are considered for analysis.
Following medicines are frequently prescribed in SLE – Thuja Occ, Staph, Apis Mel, Graphitis, Ars Alb, Kali Bi, Calc C, etc.
We don’t encourage patients to experiment with homoeopathic medications. Self-prescription can prove harmful, and parents are not encouraged to self-prescribe any of the Homeopathic medicines without consulting an appropriately qualified doctor from a recognized university.
Let our team of Let’s homoeopathy help you fight this disease. We should remember that these illnesses are not taboo – these just as any other medical problem.
So, do not hesitate and waste more time! Get a consultation with a qualified and experienced Homeopath today from the comfort of your home through Let’s Homeopathy. We will deliver the medicines to your doorstep too!